Heel Ache
Overview

The most common cause of heel pain is inflammation due to injury of the soft tissue around your heel. The plantar fascia is the area of your foot most likely to be inflamed, which results in plantar fasciitis. With plantar fasciitis, you experience a sharp burning or stabbing sensation upon arising after walking or standing for prolonged periods. Your first steps each morning probably hurt, too. Heel pain is occasionally caused by excessive pounding on the heels. This is more common in the elderly and overweight individuals whose heel fat pads no longer function properly. Watch for a bruising sensation under the heel when standing and walking. If you think this is your issue, an insert with an artificial fat pad might help alleviate your discomfort. Heel pain is by far the most common foot complaint. There are many medical conditions that are associated with heel pain, including gout and other forms of arthritis.
Causes
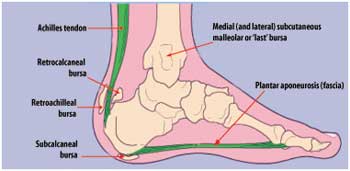
Common causes of heel pain include, Heel Spurs, a bony growth on the underside of the heel bone. The spur, visible by X-ray, appears as a protrusion that can extend forward as much as half an inch. When there is no indication of bone enlargement, the condition is sometimes referred to as "heel spur syndrome." Heel spurs result from strain on the muscles and ligaments of the foot, by stretching of the long band of tissue that connects the heel and the ball of the foot, and by repeated tearing away of the lining or membrane that covers the heel bone. These conditions may result from biomechanical imbalance, running or jogging, improperly fitted or excessively worn shoes, or obesity. Plantar Fasciitis, both heel pain and heel spurs are frequently associated with plantar fasciitis, an inflammation of the band of fibrous connective tissue (fascia) running along the bottom (plantar surface) of the foot, from the heel to the ball of the foot. It is common among athletes who run and jump a lot, and it can be quite painful. The condition occurs when the plantar fascia is strained over time beyond its normal extension, causing the soft tissue fibers of the fascia to tear or stretch at points along its length; this leads to inflammation, pain, and possibly the growth of a bone spur where the plantar fascia attaches to the heel bone. The inflammation may be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation that sometimes accompanies an athletic lifestyle. Resting provides only temporary relief. When you resume walking, particularly after a night's sleep, you may experience a sudden elongation of the fascia band, which stretches and pulls on the heel. As you walk, the heel pain may lessen or even disappear, but that may be just a false sense of relief. The pain often returns after prolonged rest or extensive walking. Heel pain sometimes results from excessive pronation. Pronation is the normal flexible motion and flattening of the arch of the foot that allows it to adapt to ground surfaces and absorb shock in the normal walking pattern. As you walk, the heel contacts the ground first; the weight shifts first to the outside of the foot, then moves toward the big toe. The arch rises, the foot generally rolls upward and outward, becoming rigid and stable in order to lift the body and move it forward. Excessive pronation-excessive inward motion-can create an abnormal amount of stretching and pulling on the ligaments and tendons attaching to the bottom back of the heel bone. Excessive pronation may also contribute to injury to the hip, knee, and lower back. Pain at the back of the heel is associated with Achilles tendinitis, which is inflammation of the Achilles tendon as it runs behind the ankle and inserts on the back surface of the heel bone. It is common among people who run and walk a lot and have tight tendons. The condition occurs when the tendon is strained over time, causing the fibers to tear or stretch along its length, or at its insertion on to the heel bone. This leads to inflammation, pain, and the possible growth of a bone spur on the back of the heel bone. The inflammation is aggravated by the chronic irritation that sometimes accompanies an active lifestyle and certain activities that strain an already tight tendon. Other possible causes of heel pain include rheumatoid arthritis and other forms of arthritis, including gout, which usually manifests itself in the big toe joint, an inflamed bursa (bursitis), a small, irritated sac of fluid; a neuroma (a nerve growth); or other soft-tissue growth. Such heel pain may be associated with a heel spur or may mimic the pain of a heel spur. Haglund's deformity ("pump bump"), a bone enlargement at the back of the heel bone in the area where the Achilles tendon attaches to the bone. This sometimes painful deformity generally is the result of bursitis caused by pressure against the shoe and can be aggravated by the height or stitching of a heel counter of a particular shoe, a bone bruise or contusion, which is an inflammation of the tissues that cover the heel bone. A bone bruise is a sharply painful injury caused by the direct impact of a hard object or surface on the foot.
Symptoms
Pain in the heel can be caused by many things. The commonest cause is plantar fascitis. Other causes include, being overweight, constantly being on your feet, especially on a hard surface like concrete and wearing hard-soled footwear, thinning or weakness of the fat pads of the heel, injury to the bones or padding of the heel, arthritis in the ankle or heel (subtalar) joint, irritation of the nerves on the inner or outer sides of the heel, fracture of the heel bone (calcaneum).
Diagnosis
After you have described your foot symptoms, your doctor will want to know more details about your pain, your medical history and lifestyle, including. Whether your pain is worse at specific times of the day or after specific activities. Any recent injury to the area. Your medical and orthopedic history, especially any history of diabetes, arthritis or injury to your foot or leg. Your age and occupation. Your recreational activities, including sports and exercise programs. The type of shoes you usually wear, how well they fit, and how frequently you buy a new pair. Your doctor will examine you, including. An evaluation of your gait. While you are barefoot, your doctor will ask you to stand still and to walk in order to evaluate how your foot moves as you walk. An examination of your feet. Your doctor may compare your feet for any differences between them. Then your doctor may examine your painful foot for signs of tenderness, swelling, discoloration, muscle weakness and decreased range of motion. A neurological examination. The nerves and muscles may be evaluated by checking strength, sensation and reflexes. In addition to examining you, your health care professional may want to examine your shoes. Signs of excessive wear in certain parts of a shoe can provide valuable clues to problems in the way you walk and poor bone alignment. Depending on the results of your physical examination, you may need foot X-rays or other diagnostic tests.
Non Surgical Treatment
Initial treatment should consist of an ice pack. Some runners prefer to use a wet towel that has been in the fridge. We recommend you use commercially available ice packs for focused pain released. An anti-inflammatory such as Ibuprofen will help to reduce the swelling. Please note this should be taken with meals and never before running. As with all soft tissue injuries, you may have to re-examine your training regime. A reduction or even a total break form running may be necessary. . Examine your running shoes, making sure the shoes do not bend excessively near the middle of the foot and at the ball of the foot. Sports shoes with built in insoles can be beneficial, however we recommend you replace existing insoles with specific sports orthotics/ insoles. Silicone heel cups, leather heel pads and contrasting cold and hot therapy can all help to speed up the healing process. The plantar fascia stretch will help to prevent the injury from occurring again. Please note that this stretch should not be done while the heel is inflamed and should only be attempted once you?re a feeling minimal or no pain from your heel.
Surgical Treatment
At most 95% of heel pain can be treated without surgery. A very low percentage of people really need to have surgery on the heel. It is a biomechanical problem and it?s very imperative that you not only get evaluated, but receive care immediately. Having heel pain is like having a problem with your eyes; as you would get glasses to correct your eyes, you should look into orthotics to correct your foot. Orthotics are sort of like glasses for the feet. They correct and realign the foot to put them into neutral or normal position to really prevent heel pain, and many other foot issues. Whether it be bunions, hammertoes, neuromas, or even ankle instability, a custom orthotic is something worth considering.
no foot pain
Prevention

A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight.

The most common cause of heel pain is inflammation due to injury of the soft tissue around your heel. The plantar fascia is the area of your foot most likely to be inflamed, which results in plantar fasciitis. With plantar fasciitis, you experience a sharp burning or stabbing sensation upon arising after walking or standing for prolonged periods. Your first steps each morning probably hurt, too. Heel pain is occasionally caused by excessive pounding on the heels. This is more common in the elderly and overweight individuals whose heel fat pads no longer function properly. Watch for a bruising sensation under the heel when standing and walking. If you think this is your issue, an insert with an artificial fat pad might help alleviate your discomfort. Heel pain is by far the most common foot complaint. There are many medical conditions that are associated with heel pain, including gout and other forms of arthritis.
Causes
Common causes of heel pain include, Heel Spurs, a bony growth on the underside of the heel bone. The spur, visible by X-ray, appears as a protrusion that can extend forward as much as half an inch. When there is no indication of bone enlargement, the condition is sometimes referred to as "heel spur syndrome." Heel spurs result from strain on the muscles and ligaments of the foot, by stretching of the long band of tissue that connects the heel and the ball of the foot, and by repeated tearing away of the lining or membrane that covers the heel bone. These conditions may result from biomechanical imbalance, running or jogging, improperly fitted or excessively worn shoes, or obesity. Plantar Fasciitis, both heel pain and heel spurs are frequently associated with plantar fasciitis, an inflammation of the band of fibrous connective tissue (fascia) running along the bottom (plantar surface) of the foot, from the heel to the ball of the foot. It is common among athletes who run and jump a lot, and it can be quite painful. The condition occurs when the plantar fascia is strained over time beyond its normal extension, causing the soft tissue fibers of the fascia to tear or stretch at points along its length; this leads to inflammation, pain, and possibly the growth of a bone spur where the plantar fascia attaches to the heel bone. The inflammation may be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation that sometimes accompanies an athletic lifestyle. Resting provides only temporary relief. When you resume walking, particularly after a night's sleep, you may experience a sudden elongation of the fascia band, which stretches and pulls on the heel. As you walk, the heel pain may lessen or even disappear, but that may be just a false sense of relief. The pain often returns after prolonged rest or extensive walking. Heel pain sometimes results from excessive pronation. Pronation is the normal flexible motion and flattening of the arch of the foot that allows it to adapt to ground surfaces and absorb shock in the normal walking pattern. As you walk, the heel contacts the ground first; the weight shifts first to the outside of the foot, then moves toward the big toe. The arch rises, the foot generally rolls upward and outward, becoming rigid and stable in order to lift the body and move it forward. Excessive pronation-excessive inward motion-can create an abnormal amount of stretching and pulling on the ligaments and tendons attaching to the bottom back of the heel bone. Excessive pronation may also contribute to injury to the hip, knee, and lower back. Pain at the back of the heel is associated with Achilles tendinitis, which is inflammation of the Achilles tendon as it runs behind the ankle and inserts on the back surface of the heel bone. It is common among people who run and walk a lot and have tight tendons. The condition occurs when the tendon is strained over time, causing the fibers to tear or stretch along its length, or at its insertion on to the heel bone. This leads to inflammation, pain, and the possible growth of a bone spur on the back of the heel bone. The inflammation is aggravated by the chronic irritation that sometimes accompanies an active lifestyle and certain activities that strain an already tight tendon. Other possible causes of heel pain include rheumatoid arthritis and other forms of arthritis, including gout, which usually manifests itself in the big toe joint, an inflamed bursa (bursitis), a small, irritated sac of fluid; a neuroma (a nerve growth); or other soft-tissue growth. Such heel pain may be associated with a heel spur or may mimic the pain of a heel spur. Haglund's deformity ("pump bump"), a bone enlargement at the back of the heel bone in the area where the Achilles tendon attaches to the bone. This sometimes painful deformity generally is the result of bursitis caused by pressure against the shoe and can be aggravated by the height or stitching of a heel counter of a particular shoe, a bone bruise or contusion, which is an inflammation of the tissues that cover the heel bone. A bone bruise is a sharply painful injury caused by the direct impact of a hard object or surface on the foot.
Symptoms
Pain in the heel can be caused by many things. The commonest cause is plantar fascitis. Other causes include, being overweight, constantly being on your feet, especially on a hard surface like concrete and wearing hard-soled footwear, thinning or weakness of the fat pads of the heel, injury to the bones or padding of the heel, arthritis in the ankle or heel (subtalar) joint, irritation of the nerves on the inner or outer sides of the heel, fracture of the heel bone (calcaneum).
Diagnosis
After you have described your foot symptoms, your doctor will want to know more details about your pain, your medical history and lifestyle, including. Whether your pain is worse at specific times of the day or after specific activities. Any recent injury to the area. Your medical and orthopedic history, especially any history of diabetes, arthritis or injury to your foot or leg. Your age and occupation. Your recreational activities, including sports and exercise programs. The type of shoes you usually wear, how well they fit, and how frequently you buy a new pair. Your doctor will examine you, including. An evaluation of your gait. While you are barefoot, your doctor will ask you to stand still and to walk in order to evaluate how your foot moves as you walk. An examination of your feet. Your doctor may compare your feet for any differences between them. Then your doctor may examine your painful foot for signs of tenderness, swelling, discoloration, muscle weakness and decreased range of motion. A neurological examination. The nerves and muscles may be evaluated by checking strength, sensation and reflexes. In addition to examining you, your health care professional may want to examine your shoes. Signs of excessive wear in certain parts of a shoe can provide valuable clues to problems in the way you walk and poor bone alignment. Depending on the results of your physical examination, you may need foot X-rays or other diagnostic tests.
Non Surgical Treatment
Initial treatment should consist of an ice pack. Some runners prefer to use a wet towel that has been in the fridge. We recommend you use commercially available ice packs for focused pain released. An anti-inflammatory such as Ibuprofen will help to reduce the swelling. Please note this should be taken with meals and never before running. As with all soft tissue injuries, you may have to re-examine your training regime. A reduction or even a total break form running may be necessary. . Examine your running shoes, making sure the shoes do not bend excessively near the middle of the foot and at the ball of the foot. Sports shoes with built in insoles can be beneficial, however we recommend you replace existing insoles with specific sports orthotics/ insoles. Silicone heel cups, leather heel pads and contrasting cold and hot therapy can all help to speed up the healing process. The plantar fascia stretch will help to prevent the injury from occurring again. Please note that this stretch should not be done while the heel is inflamed and should only be attempted once you?re a feeling minimal or no pain from your heel.
Surgical Treatment
At most 95% of heel pain can be treated without surgery. A very low percentage of people really need to have surgery on the heel. It is a biomechanical problem and it?s very imperative that you not only get evaluated, but receive care immediately. Having heel pain is like having a problem with your eyes; as you would get glasses to correct your eyes, you should look into orthotics to correct your foot. Orthotics are sort of like glasses for the feet. They correct and realign the foot to put them into neutral or normal position to really prevent heel pain, and many other foot issues. Whether it be bunions, hammertoes, neuromas, or even ankle instability, a custom orthotic is something worth considering.
no foot pain
Prevention

A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight.
What Are Fallen Arches
Overview
They make it possible for us to walk, run, and stand. With over two dozen bones, your feet are really a masterpiece of engineering. But sometimes even the best made things have flaws. One common problem is to have flatfeet, or fallen arches.
Causes
Family history, experts say fallen arches can run in families. Weak arch, the arch of the foot may be there when no weight is placed on it, for example, when the person is sitting. But as soon as they stand up the foot flattens (falls) onto the ground. Injury, arthritis, tibialis posterior (ruptured tendon), pregnancy, nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Tarsal Coalition, the bones of the foot fuse together in an unusual way, resulting in stiff and flat feet. Most commonly diagnosed during childhood. Diabetes. Age and wear and tear, years of using your feet to walk, run, and jump eventually may take its toll. One of the eventual consequences could be fallen arches. The posterior tibial tendon may become weakened after long-term wear a tear. The postario tibial tendon is the main support structure of the arch of our feet. The tendon can become inflamed (tendinitis) after overuse - sometimes it can even become torn. Once the tendon is damaged, the arch shape of the foot may flatten.
Symptoms
The primary symptom of fallen arches is painful or achy feet in the area in which the foot arches or on the heel. This area may become swollen and painful to stand still on. This causes the patient to improperly balance on their feet which in turn will cause other biomechanical injuries such as back, leg and knee pain.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
no-foot-pain.com
Non Surgical Treatment
Treatment in adults generally consists of wearing spacious, comfortable shoes with good arch support. Your doctor may recommend padding for the heel (heel cup) or orthotic shoe devices, which are molded pieces of rubber, leather, metal, plastic, or other synthetic material that are inserted into a shoe. They balance the foot in a neutral position and cushion the foot from excessive pounding. For children, treatment using corrective shoes or inserts is rarely needed, as the arch usually develops normally by age 5.
Surgery is rarely needed.
Surgical Treatment

Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Flatfeet in children are often an inherited family trait, but it may be possible to prevent the condition in some cases. Recent research has shown that there are several social or cultural factors that can cause flatfeet. These factors include the following, obesity, overweight, unnecessary orthopedic treatments, wearing rigid shoes at a young age, In 1992, a study in India of 2300 children aged 4-13 demonstrated a significant difference in the rate of flatfeet among those who wore shoes regularly and those who did not. In this study, wearing inflexible, closed-toe shoes in early childhood was shown to have a negative effect on the normal development of arches. Children who were allowed to go barefoot or who wore light sandals and slippers had a much lower rate of flatfeet. In 1999, a study in Spain of 1181 children aged 4-13 revealed that the use of orthopedic shoes for treatment of flatfeet in children not only failed to correct the problem, but actually worsened the condition by preventing the normal flexing and arch development of bare or lightly protected feet. Finally, in 2006, a study of 835 children aged 3-6 showed significant differences in the rate of flatfeet based on weight, with normal-weight children having lower rates of flatfeet than children who were overweight or obese. Among adults, flatfeet due to injury, disease, or normal aging are not preventable. However, when flatfeet are related to lifestyle factors, such as physical activities, shoe selection, and weight gain, careful attention to these factors may prevent the development of flatfeet.
They make it possible for us to walk, run, and stand. With over two dozen bones, your feet are really a masterpiece of engineering. But sometimes even the best made things have flaws. One common problem is to have flatfeet, or fallen arches.
Causes
Family history, experts say fallen arches can run in families. Weak arch, the arch of the foot may be there when no weight is placed on it, for example, when the person is sitting. But as soon as they stand up the foot flattens (falls) onto the ground. Injury, arthritis, tibialis posterior (ruptured tendon), pregnancy, nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida. Tarsal Coalition, the bones of the foot fuse together in an unusual way, resulting in stiff and flat feet. Most commonly diagnosed during childhood. Diabetes. Age and wear and tear, years of using your feet to walk, run, and jump eventually may take its toll. One of the eventual consequences could be fallen arches. The posterior tibial tendon may become weakened after long-term wear a tear. The postario tibial tendon is the main support structure of the arch of our feet. The tendon can become inflamed (tendinitis) after overuse - sometimes it can even become torn. Once the tendon is damaged, the arch shape of the foot may flatten.
Symptoms
The primary symptom of fallen arches is painful or achy feet in the area in which the foot arches or on the heel. This area may become swollen and painful to stand still on. This causes the patient to improperly balance on their feet which in turn will cause other biomechanical injuries such as back, leg and knee pain.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
no-foot-pain.com
Non Surgical Treatment
Treatment in adults generally consists of wearing spacious, comfortable shoes with good arch support. Your doctor may recommend padding for the heel (heel cup) or orthotic shoe devices, which are molded pieces of rubber, leather, metal, plastic, or other synthetic material that are inserted into a shoe. They balance the foot in a neutral position and cushion the foot from excessive pounding. For children, treatment using corrective shoes or inserts is rarely needed, as the arch usually develops normally by age 5.
Surgery is rarely needed.
Surgical Treatment

Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Flatfeet in children are often an inherited family trait, but it may be possible to prevent the condition in some cases. Recent research has shown that there are several social or cultural factors that can cause flatfeet. These factors include the following, obesity, overweight, unnecessary orthopedic treatments, wearing rigid shoes at a young age, In 1992, a study in India of 2300 children aged 4-13 demonstrated a significant difference in the rate of flatfeet among those who wore shoes regularly and those who did not. In this study, wearing inflexible, closed-toe shoes in early childhood was shown to have a negative effect on the normal development of arches. Children who were allowed to go barefoot or who wore light sandals and slippers had a much lower rate of flatfeet. In 1999, a study in Spain of 1181 children aged 4-13 revealed that the use of orthopedic shoes for treatment of flatfeet in children not only failed to correct the problem, but actually worsened the condition by preventing the normal flexing and arch development of bare or lightly protected feet. Finally, in 2006, a study of 835 children aged 3-6 showed significant differences in the rate of flatfeet based on weight, with normal-weight children having lower rates of flatfeet than children who were overweight or obese. Among adults, flatfeet due to injury, disease, or normal aging are not preventable. However, when flatfeet are related to lifestyle factors, such as physical activities, shoe selection, and weight gain, careful attention to these factors may prevent the development of flatfeet.
Leg Length Discrepancy Surgical Treatment
Overview
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
Causes
LLDs are very common. Sometimes the cause isn?t known. But the known causes of LLD in children include, injury or infection that slows growth of one leg bone. Injury to the growth plate (a soft part of a long bone that allows the bone to grow). Growth plate injury can slow bone growth in that leg. Fracture to a leg bone that causes overgrowth of the bone as it heals. A congenital (present at birth) problem (one whole side of the child?s body may be larger than the other side). Conditions that affect muscles and nerves, such as polio.
Symptoms
The patient/athlete may present with an altered gait (such as limping) and/or scoliosis and/or low back pain. Lower extremity disorders are possibly associated with LLD, some of these are increased hip pain and degeneration (especially involving the long leg). Increased risk of: knee injury, ITB syndrome, pronation and plantar fascitis, asymmetrical strength in lower extremity. Increased disc or vertebral degeneration. Symptoms vary between patients, some patients may complain of just headaches.
Diagnosis
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
Heel lifts Raise the heel on the shorter leg. It is applied either to the heel of the custom orthotic or to the inside of the shoe under the insole at the heel. Generally if the discrepancy is greater than 3/8 of an inch, the modification is applied externally on the footwear. Custom made orthotics help to provide proper support and alignment to the foot, controlling conditions such as over pronation. Orthopedic Footwear, properly fitted, to which a lift might be applied inside or out.

how we can increase our height?
Surgical Treatment
In growing children, legs can be made equal or nearly equal in length with a relatively simple surgical procedure. This procedure slows down the growth of the longer leg at one or two growth sites. Your physician can tell you how much equalization can be gained by this procedure. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the limb length discrepancy will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical. The goal is to reach equal leg length by the time growth normally ends. This is usually in the mid-to-late teenage years. Disadvantages of this option include the possibility of slight over-correction or under-correction of the limb length discrepancy. In addition, the patient's adult height will be less than if the shorter leg had been lengthened. Correction of significant limb length discrepancy by this method may make a patient's body look slightly disproportionate because of the shorter leg. In some cases the longer leg can be shortened, but a major shortening may weaken the muscles of the leg. In the thighbone (femur), a maximum of 3 inches can be shortened. In the shinbone, a maximum of 2 inches can be shortened.
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.

Causes
LLDs are very common. Sometimes the cause isn?t known. But the known causes of LLD in children include, injury or infection that slows growth of one leg bone. Injury to the growth plate (a soft part of a long bone that allows the bone to grow). Growth plate injury can slow bone growth in that leg. Fracture to a leg bone that causes overgrowth of the bone as it heals. A congenital (present at birth) problem (one whole side of the child?s body may be larger than the other side). Conditions that affect muscles and nerves, such as polio.
Symptoms
The patient/athlete may present with an altered gait (such as limping) and/or scoliosis and/or low back pain. Lower extremity disorders are possibly associated with LLD, some of these are increased hip pain and degeneration (especially involving the long leg). Increased risk of: knee injury, ITB syndrome, pronation and plantar fascitis, asymmetrical strength in lower extremity. Increased disc or vertebral degeneration. Symptoms vary between patients, some patients may complain of just headaches.
Diagnosis
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
Heel lifts Raise the heel on the shorter leg. It is applied either to the heel of the custom orthotic or to the inside of the shoe under the insole at the heel. Generally if the discrepancy is greater than 3/8 of an inch, the modification is applied externally on the footwear. Custom made orthotics help to provide proper support and alignment to the foot, controlling conditions such as over pronation. Orthopedic Footwear, properly fitted, to which a lift might be applied inside or out.

how we can increase our height?
Surgical Treatment
In growing children, legs can be made equal or nearly equal in length with a relatively simple surgical procedure. This procedure slows down the growth of the longer leg at one or two growth sites. Your physician can tell you how much equalization can be gained by this procedure. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the limb length discrepancy will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical. The goal is to reach equal leg length by the time growth normally ends. This is usually in the mid-to-late teenage years. Disadvantages of this option include the possibility of slight over-correction or under-correction of the limb length discrepancy. In addition, the patient's adult height will be less than if the shorter leg had been lengthened. Correction of significant limb length discrepancy by this method may make a patient's body look slightly disproportionate because of the shorter leg. In some cases the longer leg can be shortened, but a major shortening may weaken the muscles of the leg. In the thighbone (femur), a maximum of 3 inches can be shortened. In the shinbone, a maximum of 2 inches can be shortened.
Mortons Neuroma Causes
Overview
 Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.
Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.
Causes
The pain of Morton's neuroma occurs when the nerve connecting the toe bones (metatarsal bones) becomes irritated or compressed. The exact cause of the irritation is unknown, but it may be the metatarsal bones pressing against the nerve when the gap between the bones is narrow. This causes the nerve and surrounding tissue to thicken. Some experts believe that a number of other foot problems, including flat feet, high foot arches, bunions and hammer toes, may also play a role in Morton's neuroma.
Symptoms
If you have a Morton?s neuroma, you may have one or more of these symptoms where the nerve damage is occurring, Tingling, burning, or numbness, pain, a feeling that something is inside the ball of the foot or a feeling that there?s something in the shoe or a sock is bunched up. The progression of a Morton?s neuroma often follows the following pattern. The symptoms begin gradually. At first they occur only occasionally, when wearing narrow-toed shoes or performing certain aggravating activities. The symptoms may go away temporarily by removing the shoe, massaging the foot, or by avoiding aggravating shoes or activities. Over time the symptoms progressively worsen and may persist for several days or weeks. The symptoms become more intense as the neuroma enlarges and the temporary changes in the nerve become permanent.
Diagnosis
The most common condition misdiagnosed as Morton's neuroma is metatarsophalangeal (MTP) joint synovitis. When pain occurs in the third interspace, the clinician may misdiagnose the condition as Morton's neuroma instead of MTP synovitis, which may manifest very much like Morton's neuroma. MTP synovitis is distinguished from Morton's neuroma by subtle swelling around the joint, pain localized mainly within the joint, and pain with forced toe flexion. Palpation of the MTP joint is performed best with a pinching maneuver from the dorsal and plantar aspects of the joint to elicit tenderness of the joint. Other conditions often misdiagnosed as Morton's neuroma include the following. Stress fracture of the neck of the metatarsal. Rheumatoid arthritis and other systemic arthritic conditions. Hammertoe. Metatarsalgia (ie, plantar tenderness over the metatarsal head) Less common conditions that have overlapping symptoms with Morton's neuroma include the following. Neoplasms. Metatarsal head osteonecrosis. Freiburg. steochondrosis. Ganglion cysts. Intermetatarsal bursal fluid collections. True neuromas.
Non Surgical Treatment
The first step in treating Morton's Neuroma is to select proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating and relieving the pain. The next step in treatment is to use an orthotic designed with a metatarsal pad. This pad is located behind the ball-of-the-foot to unload pressure, and relieve the pain caused by the neuroma.
If problem persists, consult your foot doctor.
Surgical Treatment
If symptoms do not respond to any of the above measures then surgery may be suggested. This involves a short 30 minute operation to either remove tissue to take pressure off the nerve or to remove the nerve causing the pain. The surgery can be done as a day case but it will be two or three weeks before you can be fully active on your feet. There may be some lingering numbness afterwards if the nerve is removed. But surgery is successful in around 80% of cases. There is a small risk of complications such as infection and thickening of the skin on the soles of the feet.
 Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.
Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.Causes
The pain of Morton's neuroma occurs when the nerve connecting the toe bones (metatarsal bones) becomes irritated or compressed. The exact cause of the irritation is unknown, but it may be the metatarsal bones pressing against the nerve when the gap between the bones is narrow. This causes the nerve and surrounding tissue to thicken. Some experts believe that a number of other foot problems, including flat feet, high foot arches, bunions and hammer toes, may also play a role in Morton's neuroma.
Symptoms
If you have a Morton?s neuroma, you may have one or more of these symptoms where the nerve damage is occurring, Tingling, burning, or numbness, pain, a feeling that something is inside the ball of the foot or a feeling that there?s something in the shoe or a sock is bunched up. The progression of a Morton?s neuroma often follows the following pattern. The symptoms begin gradually. At first they occur only occasionally, when wearing narrow-toed shoes or performing certain aggravating activities. The symptoms may go away temporarily by removing the shoe, massaging the foot, or by avoiding aggravating shoes or activities. Over time the symptoms progressively worsen and may persist for several days or weeks. The symptoms become more intense as the neuroma enlarges and the temporary changes in the nerve become permanent.
Diagnosis
The most common condition misdiagnosed as Morton's neuroma is metatarsophalangeal (MTP) joint synovitis. When pain occurs in the third interspace, the clinician may misdiagnose the condition as Morton's neuroma instead of MTP synovitis, which may manifest very much like Morton's neuroma. MTP synovitis is distinguished from Morton's neuroma by subtle swelling around the joint, pain localized mainly within the joint, and pain with forced toe flexion. Palpation of the MTP joint is performed best with a pinching maneuver from the dorsal and plantar aspects of the joint to elicit tenderness of the joint. Other conditions often misdiagnosed as Morton's neuroma include the following. Stress fracture of the neck of the metatarsal. Rheumatoid arthritis and other systemic arthritic conditions. Hammertoe. Metatarsalgia (ie, plantar tenderness over the metatarsal head) Less common conditions that have overlapping symptoms with Morton's neuroma include the following. Neoplasms. Metatarsal head osteonecrosis. Freiburg. steochondrosis. Ganglion cysts. Intermetatarsal bursal fluid collections. True neuromas.
Non Surgical Treatment
The first step in treating Morton's Neuroma is to select proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating and relieving the pain. The next step in treatment is to use an orthotic designed with a metatarsal pad. This pad is located behind the ball-of-the-foot to unload pressure, and relieve the pain caused by the neuroma.
If problem persists, consult your foot doctor.

Surgical Treatment
If symptoms do not respond to any of the above measures then surgery may be suggested. This involves a short 30 minute operation to either remove tissue to take pressure off the nerve or to remove the nerve causing the pain. The surgery can be done as a day case but it will be two or three weeks before you can be fully active on your feet. There may be some lingering numbness afterwards if the nerve is removed. But surgery is successful in around 80% of cases. There is a small risk of complications such as infection and thickening of the skin on the soles of the feet.
For Leg Length Imbalances Chiropodists Prefer Shoe Lifts
There are two unique variations of leg length discrepancies, congenital and acquired. Congenital means you are born with it. One leg is anatomically shorter than the other. Through developmental phases of aging, the human brain picks up on the walking pattern and recognizes some variance. The human body typically adapts by dipping one shoulder to the "short" side. A difference of less than a quarter inch is not blatantly uncommon, does not need Shoe Lifts to compensate and in most cases doesn't have a profound effect over a lifetime.

Leg length inequality goes largely undiscovered on a daily basis, yet this problem is easily remedied, and can eradicate numerous cases of chronic back pain.
Treatment for leg length inequality commonly consists of Shoe Lifts . Many are economical, generally being under twenty dollars, compared to a custom orthotic of $200 or maybe more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Low back pain is easily the most widespread health problem affecting men and women today. Around 80 million people are afflicted by back pain at some point in their life. It is a problem which costs businesses vast amounts of money year after year on account of time lost and production. New and improved treatment solutions are continually sought after in the hope of decreasing the economical impact this condition causes.

Men and women from all corners of the world suffer the pain of foot ache due to leg length discrepancy. In a lot of these situations Shoe Lifts are usually of very beneficial. The lifts are capable of easing any pain in the feet. Shoe Lifts are recommended by many professional orthopaedic physicians.
To be able to support the body in a well-balanced manner, feet have got a critical task to play. Despite that, it's often the most overlooked area in the body. Some people have flat-feet which means there may be unequal force placed on the feet. This causes other areas of the body like knees, ankles and backs to be affected too. Shoe Lifts ensure that ideal posture and balance are restored.

Leg length inequality goes largely undiscovered on a daily basis, yet this problem is easily remedied, and can eradicate numerous cases of chronic back pain.
Treatment for leg length inequality commonly consists of Shoe Lifts . Many are economical, generally being under twenty dollars, compared to a custom orthotic of $200 or maybe more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Low back pain is easily the most widespread health problem affecting men and women today. Around 80 million people are afflicted by back pain at some point in their life. It is a problem which costs businesses vast amounts of money year after year on account of time lost and production. New and improved treatment solutions are continually sought after in the hope of decreasing the economical impact this condition causes.

Men and women from all corners of the world suffer the pain of foot ache due to leg length discrepancy. In a lot of these situations Shoe Lifts are usually of very beneficial. The lifts are capable of easing any pain in the feet. Shoe Lifts are recommended by many professional orthopaedic physicians.
To be able to support the body in a well-balanced manner, feet have got a critical task to play. Despite that, it's often the most overlooked area in the body. Some people have flat-feet which means there may be unequal force placed on the feet. This causes other areas of the body like knees, ankles and backs to be affected too. Shoe Lifts ensure that ideal posture and balance are restored.
What May Cause Inferior Calcaneal Spur
:origin()/pre06/c787/th/pre/i/2005/205/0/1/feathered_rino_lizard_by_calcaneus.jpg)
Overview
A heel spur is a painful condition that is caused by the accumulation of excessive calcium under the heel of the foot. The heel bone is made up of a large structure called the calcaneus, which is connected to the bottom of the foot by durable connective tissue called fascia. If the layers of connective tissue become damaged or begin to degenerate due to wear and tear, plantar fasciitis may develop. This causes calcification, which refers to the abnormal buildup of calcium on the heel bone. As the calcium continues to accumulate, a calcified protrusion called a spur may become visible on an X-ray.
Causes
Causes of Heel Spur Syndrome are mostly due to your foot structure. Foot structure is due to hereditary for the most part, meaning it was the way you were when born. Other factors such as increase in weight, injury, improper shoes, or different activities may change the way your foot functions as well. If one leg is longer or shorter than the other, this may make your foot function improperly and be the cause of the heel spur syndrome. Improper shoes may be ones that are new or ones that are worn out and do not give good support. The higher priced shoes do not mean it's a better shoe. Pronation is a term used to describe a foot which allows the arch to fall more than normal and allows for the fascia along the bottom of the foot to put a tighter pull or a different angle of pull on the heel bone. Over time, this constant pull of the tight fascia can force the bone to enlarge and form a spur. It is not the heel spur that causes the pain directly. The spur may cause pressure against a nearby nerve causing a neuritis, or a bursa causing a bursitis.

Symptoms
It is important to be aware that heel spurs may or may not cause symptoms. Symptoms are usually related to the plantar fasciitis. You may experience significant pain and it may be worse in the morning when you first wake up or during certain physical activities such as, walking, jogging, or running.
Diagnosis
A thorough history and physical exam is always necessary for the proper diagnosis of heel spurs and other foot conditions. X rays of the heel area are helpful, as excess bone production will be visible.
Non Surgical Treatment
Heel spurs and plantar fasciitis are treated by measures that decrease the associated inflammation and avoid reinjury. Local ice applications both reduce pain and inflammation. Physical therapy methods, including stretching exercises, are used to treat and prevent plantar fasciitis. Anti-inflammatory medications, such as ibuprofen or injections of cortisone, are often helpful. Orthotic devices or shoe inserts are used to take pressure off plantar spurs (donut-shaped insert), and heel lifts can reduce stress on the Achilles tendon to relieve painful spurs at the back of the heel. Similarly, sports running shoes with soft, cushioned soles can be helpful in reducing irritation of inflamed tissues from both plantar fasciitis and heel spurs. Infrequently, surgery is performed on chronically inflamed spurs.
Surgical Treatment
Almost 90% of the people suffering from heel spur get better with nonsurgical treatments. However, if the conservative treatments do not help you and you still have pain even after 9 to 12 months, your doctor may advise surgery for treating heel spur. The surgery helps in reducing the pain and improving your mobility. Some of the surgical techniques used by doctors are release of the plantar fascia. Removal of a spur. Before the surgery, the doctor will go for some pre-surgical tests and exams. After the operation, you will need to follow some specific recommendations which may include elevation of the foot, waiting time only after which you can put weight on the foot etc.
What Is Heel Spur
Overview
The plantar fascia is connective tissue on the sole of your foot. When the arch of the foot is not properly supported, the plantar fascia can stretch and pull away from the heel area. When the plantar fascia pulls away from the heel, calcium deposits form in its absence. These calcium deposits are called heel spurs and can be very painful.
Causes
Fctors that increase the risk of developing heel spurs include a high body mass index (BMI), regular vigorous activity, and intensive training routines or sports. Factors such as these are believed to increase the incidence of repetitive stress injuries that are associated with the formation of heel spurs. When a heel spur forms, extremely sharp pain along with the feeling that a part of the heel is trying to burst through the skin usually occurs. If left untreated, an individual may eventually begin to struggle to perform simple activities such as walking.

Symptoms
Heel spurs often do not show any symptoms. If you have intermittent or chronic pain when you walk, run or jog, it may be heel spur. There will be inflammation the point where spur formation happens. The pain is caused by soft tissue injury in the heel. Patients often describe the pain as a pin or knife sticking to the heel. The pain is more specially in the morning when the patient stands up for the first time.
Diagnosis
Your doctor will discuss your medical history and will examine your foot and heel for any deformities and inflammation (swelling, redness, heat, pain). He/she will analyze your flexibility, stability, and gait (the way you walk). Occasionally an x-ray or blood tests (to rule out diseases or infections) may be requested.
Non Surgical Treatment
Get some rest. You need to stay off of your aching foot as much as possible for at least a week. Think about possible causes of the problem while you're resting and figure out how you can make some changes. Some actions that can contribute to heel spurs include running too often or running on hard surfaces such as concrete, tight calf muscles, shoes with poor shock absorption. Ease back into your activities. In many cases, you'll be in too much pain to go ahead with a strenuous exercise routine that puts pressure or impact on your heel. Listen to your body and switch to different activities such as swimming or riding a bike until your heel spurs improve.
Surgical Treatment
When chronic heel pain fails to respond to conservative treatment, surgical treatment may be necessary. Heel surgery can provide relief of pain and restore mobility. The type of procedure used is based on examination and usually consists of releasing the excessive tightness of the plantar fascia, called a plantar fascia release. Depending on the presence of excess bony build up, the procedure may or may not include removal of heel spurs. Similar to other surgical interventions, there are various modifications and surgical enhancements regarding surgery of the heel.